Research Roundup – February 2023
From promising Marburg vaccine results to an avian influenza outbreak, we bring you the latest infectious disease research and news
Leap of Faith
A recent avian influenza H5N1 outbreak on a mink farm in Galicia, Spain, has sparked concern that the virus could eventually spread to humans (1). H5N1 has increasingly been able to jump from birds to mammals in recent years, but so far these infections were caused by the mammals coming into direct contact with virus-contaminated material. This current spread between mammals indicates that H5N1 might be a bigger threat to public health than previously thought – prompting calls for more precautionary measures to mitigate the public health risk.
New Developments
A small first-in-human trial of the cAd3-Marburg vaccine has revealed it has good safety, tolerability, and immunogenicity – showing similar safety to that of cAd3-vectored filovirus vaccines (2). At four weeks post-vaccination, 95 percent of participants yielded a glycoprotein-specific antibody response. By 48 weeks, 70 percent of vaccinees had retained this response. Given the current Marburg virus outbreak in Equatorial Guinea and the fact that there are currently no approved vaccines for the virus, the research represents a particularly promising step in the right direction.
Shaken, Not Stirred
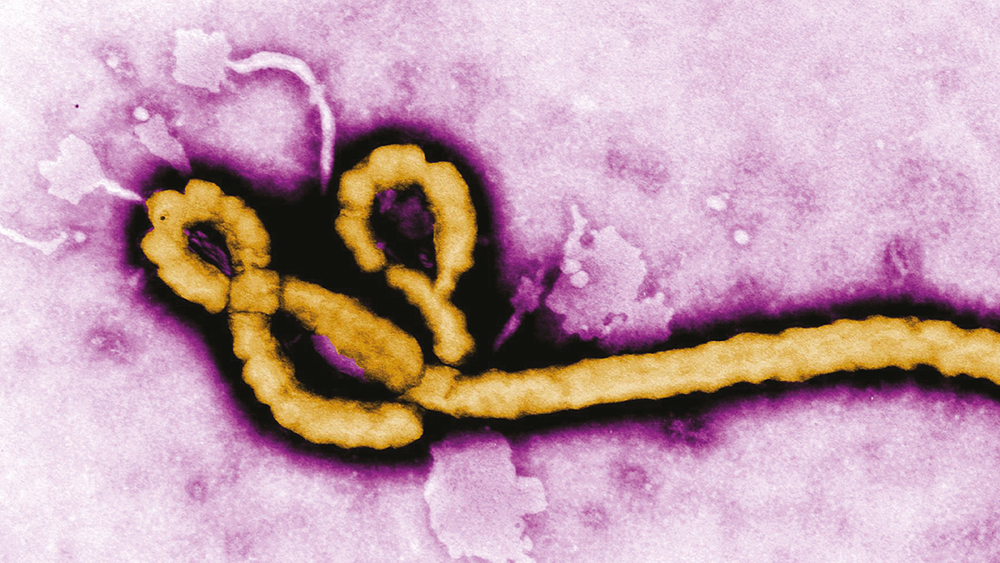
Inmazeb was first approved by the FDA to treat Zaire ebolavirus in 2020, targeting the glycoprotein on the virus’ surface. In a new study, researchers have described the cryo-EM structure of the three-antibody cocktail, with the high-resolution, 3D structure showing how the three antibodies bind to ebolavirus glycoprotein (3). They also demonstrate how, unlike monotherapies (even those targeting conserved epitopes), Inmazeb protects against rapidly emerging ebolavirus escape mutants. Overall, the results support the benefit of a combination approach over monotherapy.
Future Formulation
Researchers have tested an in-situ forming implant (ISFI) that can release ultra-long-acting cabotegravir (CAB) in female mice and macaques (4). CAB ISFI extends dosing intervals and provides durable protection against rectal SHIV infection in female macaques. The formulation can release CAB for 6–11 months at levels above established benchmarks for PrEP protection in macaques and humans – what’s more, the implant can be retrieved and removed. Based on the results, the authors suggest that the formulation shows potential for clinical administration two to three times per year – providing expanded preventative options for people living with HIV who might not want to take daily medication.
Lessons Learned
Experts have reviewed the National Institutes of Health’s research response to COVID-19, highlighting key milestones and lessons learned (5). The initiatives reviewed include investing in vaccine development and evaluation; building diversity in clinical trials; prioritizing therapeutic trials; and streamlining diagnostics development. The authors highlight the need for ongoing global surveillance to deal with emerging pathogens and better communication systems to empower trusted sources and combat misinformation. They also advocate for the importance of collective collaboration and continuous investment in basic and applied research.
References
- SM Sidik, “Bird flu outbreak in mink sparks concern about spread in people” (2023). Available at: go.nature.com/3YDUVQ4.
- MJ Hamer et al., “Safety, tolerability, and immunogenicity of the chimpanzee adenovirus type 3-vectored Marburg virus (cAd3-Marburg) vaccine in healthy adults in the USA: a first-in-human, phase 1, open-label, dose-escalation trial,” Lancet, 401, 294 (2023). PMID: 36709074.
- V Rayaprolu et al., “Structure of the Inmazeb cocktail and resistance to Ebola virus escape,” Cell Host Microbe, 31, 260 (2023). PMID: 36708708.
- IC Young et al., “Ultra-long-acting in-situ forming implants with cabotegravir protect female macaques against rectal SHIV infection,” Nat Commun, 14, 708 (2023). PMID: 36759645.
- F Collins et al., “The NIH-led research response to COVID-19,” Science, 379, 441 (2023). PMID: 36730407.