mRNA Vaccines: Beyond Viruses
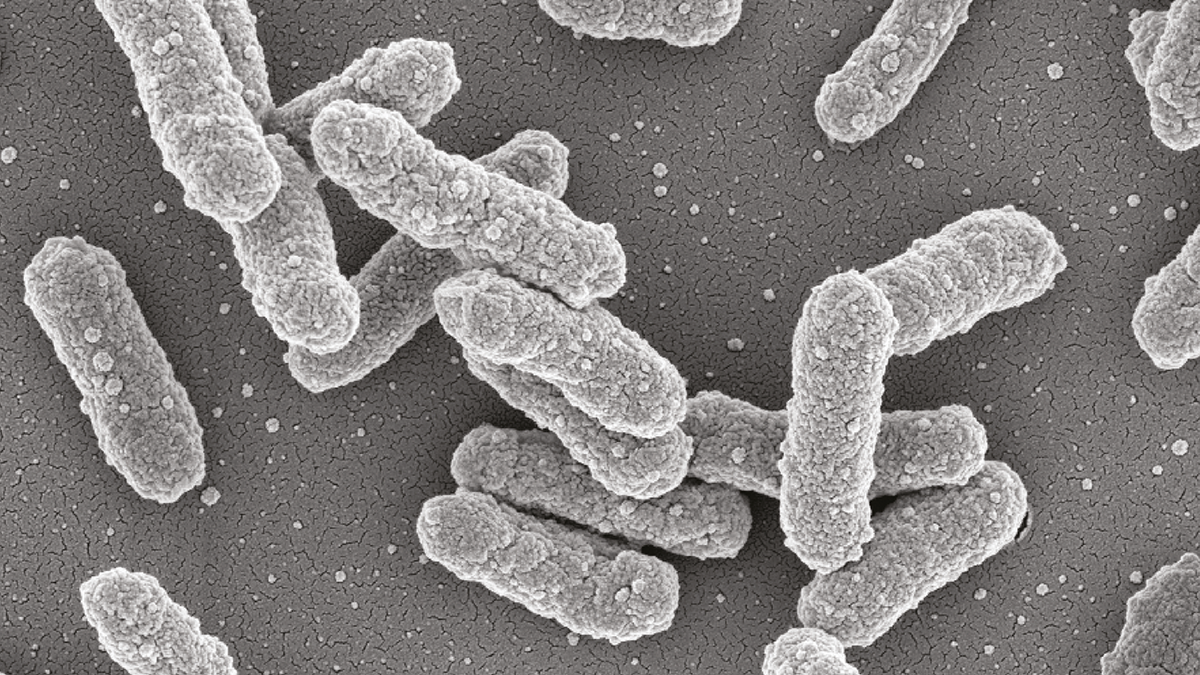
Researchers have developed a highly effective mRNA vaccine against Yersinia pestis, demonstrating mRNA’s potential against bacterial pathogens
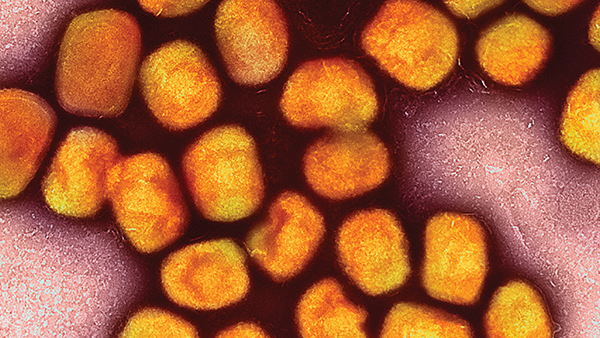
Although plenty of research focused on mRNA technology before 2020, it wasn’t until SARS-CoV-2 spread through the population that mRNA-based vaccines took center stage, with an unsurprising focus on viral pathogens. But with antimicrobial resistance plaguing already strained health systems, could mRNA vaccines offer new routes for treating – and preventing – bacterial infections?
For the first time, researchers have successfully developed an mRNA lipid nanoparticle (LNP) vaccine that is highly effective against a bacterial pathogen – namely, Yersinia pestis (1). To find out more, we spoke with one of the researchers, Dan Peer, Professor and Director of the Laboratory of Precision NanoMedicine at Tel Aviv University.
What inspired you to develop a mRNA-LNP vaccine against a bacterial pathogen?
Bacterial pathogens pose a great threat to human health and, though many bacterial infections can be resolved with antibiotics, the global emergence of antibiotic-resistant bacterial strains necessitates the development of alternative countermeasures. The recently approved mRNA-LNP vaccine platform has been evaluated extensively against viral pathogens, but few reports demonstrate the effectiveness of this platform against bacterial agents. Given the ability of the mRNA-LNP platform to elicit robust humoral and cellular immune responses, we hypothesized that it could be harnessed for bacterial infections.
Why did you choose Yersinia pestis for your proof of concept?
Our study was performed in close collaboration with the Israel Institute for Biological Research, which has gained tremendous knowledge and experience with various bacterial pathogens, including Y. pestis. Our motivation was that, if we successfully demonstrated the efficacy of the mRNA-LNP platform against a highly lethal bacterium such as Y. pestis, it could open new avenues toward the development of novel prophylactic approaches against other bacterial pathogens.
What are the challenges associated with developing mRNA vaccines against bacterial pathogens?
As evidenced by the limited reports regarding the efficacy of mRNA vaccines against bacterial pathogens, designing a bacterial antigen to be encoded by the mRNA vaccine is more complex than a viral antigen. Though viruses exploit the host’s translation machinery to produce their own proteins and subsequent production of virus particles, bacteria rely on their endogenous replication system, which does not involve eukaryotic pathways. Therefore, expression of a bacterial protein in mammalian cells could result in a protein which, although encoded by the same identical mRNA sequence, carries different modifications, which may alter its immunogenicity. Designing bacterial mRNA vaccines therefore requires deep understanding and molecular optimization of the relevant antigen.
Can you please summarize the main findings and lessons of your research?
In our study, we demonstrate the design of an effective mRNA vaccine against Y. pestis – the causative agent of plague. The vaccine is based on a major protective antigen, the F1 capsular protein, which was optimized to elicit robust immune responses. Through codon optimization, increased G/C content, human Fc conjugation, and removal of signal peptide, we were able to obtain very high anti-F1 IgG titers which, in the well-established plague mouse model, conferred full protection against a lethal challenge with Y. pestis. Importantly, the elicited immune responses were so robust that a single vaccination was sufficient to confer 100 percent protection.
As for lessons, I’d emphasize that the design and construction of mRNA vaccines against bacterial pathogens requires extensive adaptation and modification of the relevant antigen.
How might the target bacterium affect mRNA vaccine efficacy?
The life cycle of the bacterium is important. Intracellular bacteria are more similar to viruses in that they are capable of hiding from circulating antibodies (at least during the primary adaptive response). A cellular immune response – for example, CD8+ – is therefore crucial for successful elimination of intracellular bacteria (and viruses). Neutralizing antibodies will assist in controlling later phases of infection by blocking further spread of progeny viruses or bacteria – or during subsequent infection.
In contrast, extracellular bacteria generally do not “hide” inside host cells and are prone to binding by neutralizing antibodies. Therefore, humoral responses are generally highly effective against extracellular bacteria. One major advantage of the mRNA vaccine platform is its ability to elicit both humoral and cellular immune responses.
What are the strengths of mRNA vaccines for bacteria over traditional recombinant protein vaccines?
Compared with recombinant protein vaccines, mRNA vaccine production is relatively rapid, simple, inexpensive, and does not require cell culture and tedious purification stages. The mRNA vaccine platform also enables quick adaptation to emerging strains of the pathogen. We believe that our proof-of-concept study will pave the way for the development of additional mRNA vaccines against bacterial pathogens, especially in light of the global health threat of antibiotic resistance.
When might we see approved mRNA vaccines against bacteria, such as Y. Pestis?
In our study, we tested the ability of the mRNA vaccine to protect animals against bubonic plague; next, we aim to evaluate the vaccine’s ability to confer protection against pneumonic plague, which is the most serious form of the disease. Unlike SARS CoV-2, approval of an mRNA vaccine against Y. pestis may take a long time because plague disease is mostly sporadic and does not resemble the recent global pandemic affecting millions of people.
What are your predictions for mRNA-based vaccines for other bacteria given the success of your research so far?
We believe that the data collected in our study will facilitate the development of mRNA-based prophylaxis against additional bacterial pathogens. Although the modifications we applied to the Y. pestis antigen greatly increased its ability to induce robust immune responses, it is possible that other bacterial pathogens will require additional or different antigen alterations or sequence optimization. Therefore, the successful development of mRNA vaccines for other bacteria will require deep understanding of the pathogen’s biology and its potential antigens.
Reference
- E Kon et al., “A single-dose F1-based mRNA-LNP vaccine provides protection against the lethal plague bacterium,” Sci Adv, 9, eadg1036 (2023). PMID: 36888708.