From Mosquitoes to Medicine
Exploring the scientific and logistical hurdles of malaria vaccine development
Malaria remains one of the deadliest infectious diseases in the world, with an estimated 247 million cases and 619,000 deaths worldwide in 2021 alone. Significant progress in malaria control measures has been made over the past few decades, but only one malaria vaccine (RTS,S) is approved and currently used in endemic areas. Unfortunately, its effectiveness is limited and there are significant challenges to its implementation.
Given malaria’s devastating impact on global health, why do we still lack a more effective vaccine? The challenges faced by scientists trying to address this problem are manifold…
Genetic diversity
Malaria in humans is caused by six Plasmodium species, with P. falciparum and P. vivax causing most cases. P. falciparum is most associated with malaria illness and disease, especially in Africa where it causes about 99 percent of cases. P. vivax is a major burden of malaria disease in Central and South America. Although there is genetic diversity between each of the species, there is also a high level of genetic diversity observed within populations of P. falciparum. Much diversity has been discovered in the parasite surface antigens that would serve as vaccine antigens, raising concerns that:
- Vaccine efficacy may differ from one region to the next
- A vaccine targeting only a subset of variants may lead to the emergence of “vaccine resistant” variants able to cause disease within vaccinated communities
To address these concerns, scientists need information on the distribution of vaccine antigen polymorphisms in endemic areas. Efforts should also go into determining the possibility of vaccine-resistant variants for certain target antigens or conducting molecular surveillance to detect the appearance of resistance variants. Some of this work has been done (or is planned) for the current RTS,S vaccine targeting the parasite circumsporozoite protein (CSP).
When it comes to vaccine design, antigens known to have high levels of polymorphism might be avoided in favor of more conserved antigens. Furthermore, the development of polyvalent malaria vaccines or whole-organism vaccines may help address issues surrounding genetic diversity.
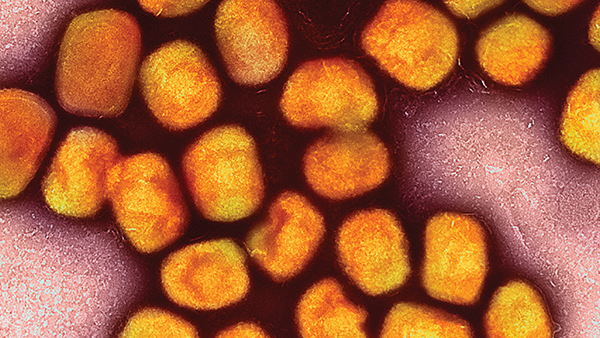
Circle of life
The complex life cycle of the malaria parasite further complicates vaccine development. Malaria parasites take on various forms during infection, making vaccine design more complex compared with bacterial and viral pathogens. The parasite genome is quite large, with more than 5,000 protein-coding genes, and each stage in the parasite life cycle is defined by unique patterns of gene expression and protein synthesis. Therefore, unlike with some pathogens, where the identification of target antigens for vaccines has been relatively straightforward (for example, spike protein for SARS-CoV-2, hemagglutinin for influenza A, pneumococcal polysaccharides), intensive research efforts have gone into identifying protein antigens to target the different stages of malaria infection. Notably, vaccines targeting these stages and unique antigens are certain to impact infection and disease differently:
- Pre-erythrocytic stage. Prevents the infection from progressing to symptomatic malaria. The main antigen of study for this vaccine type is the CSP.
- Erythrocytic stage. Controls parasite replication/levels in the individual. Major targets for this type of vaccine include the reticulocyte-binding protein homolog 5 (PfRh5), PfRh5-interacting protein (PfRipr), and glutamic-acid-rich protein (PfGARP).
- Sexual stage. Blocks the transmission and development of gametocytes from infected individuals to mosquitoes, which would work to reduce community spread of malaria. Potential target parasite antigens for this vaccine type include Pfs230, Pfs48/45, Pf25, and Pfs28.
Waning protection
The correlates of protection for both natural immunity (induced by malaria infection) and vaccine-induced immunity remain unclear. Although experimental and clinical data support both antibodies and T cells being involved in protection, the function and importance of each at the various stages of infection are not clearly defined. And that makes it challenging when trying to measure the immunogenicity of a vaccine and predict its potential protective efficacy.
As our understanding of the immune components required for protective immunity against malaria expands, developers will be better able to detect aspects of the immune response that are likely to be protective versus those that may hinder protection or cause immunopathology. For example, a few human studies have revealed an association between increased numbers of immunosuppressive regulatory T cells (Tregs) and both increased parasite numbers and disease severity. Similarly, experimental studies have demonstrated an association between increased levels of pro-inflammatory cytokines, such as TNF-α, IL-6, and IL-18, with severe illness.
To address waning efficacy over time, vaccine adjuvants can be added to malaria vaccines to enhance and prolong protective immune responses; for example, the RTS,S vaccine contains AS01, a liposome-based adjuvant. Immunity against the parasite is not durable; natural immunity resulting from infection develops slowly and wanes quickly when immune adults leave endemic areas, and data shows that frequent exposure to malaria is required to maintain immunity. Although this can be achieved through booster doses, more research is needed to identify the optimal dosing regimen that results in a robust and long-lasting immune response.
Moreover, it is likely that the immune response correlates with an individual’s age and malaria exposure history. For example, data from recent clinical trials using a live, radiation-attenuated whole organism vaccine (PfSPZ) revealed that, although vaccinated infants produced high amounts of antibodies compared with adults, antibody levels were not associated with protection against infection.
Young children suffer the greatest burden of malaria disease – with pre-existing immunity likely impacting vaccine responsiveness, immune responses in uninfected children are likely to differ from malaria-exposed adults. As such, immune correlates of protection (natural and vaccine-induced) must be identified in this population. And, as we observed with COVID-19 vaccines, vaccine antigen amounts, number of doses, and dosing regimens necessary for protection will certainly differ between children and adults.
Clinical trial conundrums
There are many questions currently left unanswered, but conducting clinical trials in regions most impacted by malaria can be challenging; many malaria-endemic countries suffer from economic, political, structural, and societal issues that hinder vaccine research and development. They also lack the resources to conduct robust and effective disease surveillance necessary for vaccine clinical trials or do not have the manufacturing capacity and expertise to produce vaccines locally. Another challenge is health literacy and vaccine hesitancy, which could be improved with funding in educational awareness campaigns in both rural and urban areas.
Vaccine misinformation resurged during COVID-19, hindering efforts to combat vaccine hesitancy and making it more challenging to recruit volunteers needed to conduct clinical trials of new malaria vaccines. In addition, the rapid development and deployment of COVID-19 vaccines dramatically changed the expectations for vaccine time-to-market and production. Much of this was due to existing basic research, investment, and significant government-industry partnerships. Similar public-private partnerships, incentive-based policies, and streamlining of clinical trials and approval processes could expedite the development of one or more effective malaria vaccines.
Not only did the pandemic reveal the risks of relying on a single or small number of approved suppliers in times of high global demand and the importance of identifying supply bottlenecks that can adversely impact development and manufacturing, it also demonstrated the critical need for trained vaccine workers. Malaria vaccine development requires individuals with expertise in testing, disease surveillance, manufacturing, distribution, and administration. The solution? Increased investment in education and workforce training, especially in low- and middle-income countries. International collaborations and partnerships should continue to be explored to help ensure equitable access to knowledge surrounding vaccine development and technologies.
The development of an effective malaria vaccine remains an urgent and ongoing priority for global health. Although progress has been made in recent years, significant challenges remain. Nonetheless, the innovative strategies and cutting-edge technologies being developed and deployed to reduce malaria burden are truly inspiring. With continued investment and collaboration, I remain hopeful that a highly effective malaria vaccine will soon become a reality – after all, such a vaccine would help eliminate this devastating disease and save countless lives around the world.
Sources
- MJ Gardner et al., “Genome sequence of the human malaria parasite Plasmodium falciparum,” Nature, 419, 498 (2002). PMID: 12368864.
- IA Cockburn, RA Seder, “Malaria prevention: from immunological concepts to effective vaccines and protective antibodies,” Nat Immunol, 19, 1199 (2018). PMID: 30333613.
- BN Kanoi et al., “Malaria vaccine approaches leveraging technologies optimized in the COVID-19 era,” Front Trop Dis, 3, 988665 (2022).
- PE Duffy, JP Gorres, “Malaria vaccines since 2000: progress, priorities, products,” NPJ Vaccines, 5, 48 (2020). PMID: 32566259.
- M Oneko et al., “Safety, immunogenicity and efficacy of PfSPZ Vaccine against malaria in infants in western Kenya: a double-blind, randomized, placebo-controlled phase 2 trial,” Nat Med, 27, 1636 (2021). PMID: 34518679.
- S Baptista et al., “COVID-19 vaccinology landscape in Africa,” Front Immunol, 13, 955168 (2022). PMID: 36544758.