You are viewing 1 of your 3 articles before login/registration is required
Dealing with a Data Deadlock
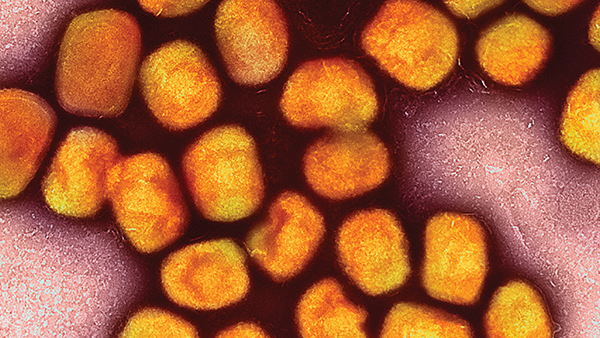
Research into WHO’s priority pathogens is booming, but it’s futile without actionable insights
Drug resistance is on the rise, and a somewhat dry pipeline of new antibiotics doesn’t paint a much rosier picture. In fact, the most recently discovered class of antibiotics was in 1987, and the FDA hasn’t approved a new antibiotic since 2019. Back in 2017, the World Health Organization (WHO) published the first ever list of antibiotic-resistant “priority pathogens,” which highlighted the 12 families of bacteria that represent the greatest threat to human health and placed them into three groups: critical, high, and medium. The list aimed to address urgent public health needs by guiding and promoting research and development of novel antibiotics. But what triggered the pipeline drought in the first place? It seems a number of issues are to blame.
“In the 1950s and 1960s, there was a huge boom in antimicrobial drug discovery, during which the ‘easy wins’ were identified,” says Thibault Géoui, Senior Director of Discovery Biology and Predictive Risk Management at Elsevier. “The challenge of finding new antibacterial compounds in the decades since has been twofold. First, investment in innovation declined due to a perceived saturation of the market in the 1990s – a time when a wide range of effective antimicrobials were available. Second, rising resistance has rendered many of the recently discovered compounds useless.”
In an effort to understand the impact of WHO’s priority pathogens list, Géoui and his team at Elsevier conducted an internal project on research activity surrounding the listed bacteria (1). Using data from Scopus, Elsevier’s abstract and citation database, they revealed that 227,808 research papers have been published on the priority pathogens since 2017, with Acinetobacter baumannii (public enemy number one) benefiting from the biggest boost in published papers between 2017 and 2021. Although Staphylococcus aureus (methicillin-resistant, vancomycin-intermediate and -resistant) rose at a slower rate over the years, the bacteria still came out on top in terms of numbers of published papers, with a whopping total of 83,165.
Certainly, research into priority pathogens is not lacking, but with such high research activity comes an even higher volume of data. Although data availability isn’t the issue, Géoui highlights a particular barrier to putting it into action. “The recent analysis shows that data on antimicrobials and the WHO’s 12 priority pathogens is increasing year-on-year and flooding the scientific domain. It is impossible for researchers in the field to read the quarter of a million articles published in the past ten years, which risks valuable insights being missed.”
Results hidden within could inform future research, help accelerate drug discovery, or simply prevent duplication of efforts – all possibly helping humanity unlock a new antibiotic. But how can we find the most informative and valuable papers – the needles in many haystacks? In an increasingly digital world, Géoui believes that artificial intelligence (AI) and related technologies could help researchers extract valuable insights from what has become big data. “Cutting-edge AI and natural language processing technologies help make sense of the information available by incorporating the data generated in experiments and published in scientific papers, along with data being held in and added to high-quality databases daily,” he says. “These technologies will accelerate drug discovery by helping to identify targets, forecast clinical side effects, and prioritize compounds of interest. During the COVID-19 pandemic, we realized the capabilities of AI in analyzing disease networks and helping to identify existing drugs which could be repurposed (2) – there is no reason a similar approach could not be employed for antimicrobial resistance.”
First, however, scientists and researchers working with priority pathogens need to be supported from the top. “The WHO has done an excellent job of raising awareness of the threat of antimicrobial resistance, but the onus is really on governments and policymakers to incentivize innovation in the field,” Géoui says. “We saw during the COVID-19 pandemic what can be achieved when public and private institutions band together to develop new therapies and know that it can be achieved. There is no arguing that drug development is expensive and, although using modern technologies to make workflows more efficient will be a part of the next phase of antimicrobial drug discovery, proper funding and incentives will be the key drivers.”
References
- PharmiWeb, “Antimicrobial Awareness Week 2022: Research into Priority Pathogens Explodes, But Now Scientists Face the Challenge of Using It,” (2022). Available at: bit.ly/3w3XXk3.
- S Richman et al., “Old drugs, new tricks: leveraging known compounds to disrupt coronavirus-induced cytokine storm,” NPJ Syst Bio Appl, 8, 38 (2022). PMID: 36216820.