All for One, One for All
How an mRNA universal flu vaccine could change the seasonal guessing
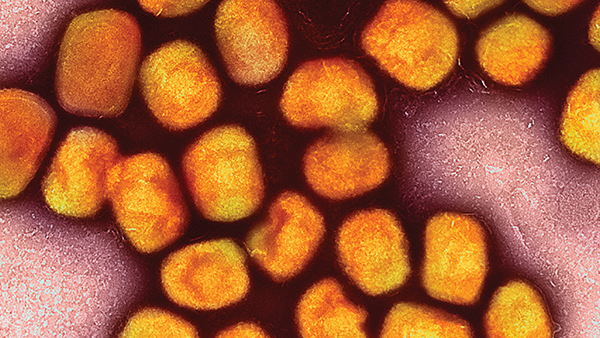
Every year, like clockwork, flu season comes a-knockin’ – and with the influenza virus’ ability to rapidly evolve, we find ourselves in a perpetual game of cat-and-mouse.
“With traditional vaccines, researchers have to identify recent mutations in the head of the HA protein and current strains that are circulating. They then develop a vaccine that will be effective against the current circulating strain of influenza,” says Wesley Farr, Lecturer at the University of West Florida and Medical Executive Director at the Florida Department of Health in Escambia County, USA.
And so, the infectious disease community dreams of a universal flu vaccine. “With an effective universal vaccine, the need for identifying mutations in the stem of the HA protein would be greatly reduced due to the stability and lower mutation rate of the stem. Although, researchers would still need to remain vigilant for the occurrence of mutations in the HA stem to maintain effectiveness of the universal vaccine.”
The theory is sound and the promise clear, but developing such a vaccine is tricky. “The main challenge is identifying a stable protein in the flu virus that will elicit antibodies that will prevent infection,” says Farr. “Not all proteins in an infectious agent do this – and expensive and time-consuming human trials are necessary to prove that a universal flu vaccine will be safe and effective.”
And yet, there is a glimmer of hope on the horizon, with the National Institutes of Health recently announcing that a phase I clinical trial for an mRNA-based universal influenza vaccine is actively recruiting volunteers (1). The study will test the safety of H1ssF-3928 mRNA-LNP and its ability to induce an immune response in healthy participants.
If successful, Farr says the benefit to individuals and public health would be manifold. “As well as eliminating the need for new vaccine development each year because it could cover all strains of seasonal influenza, it may also reduce the need for annual flu vaccinations, though the frequency of boosters will need to be determined during clinical trials and population studies during the annual flu seasons.” He continues, “A universal flu vaccine should also be effective against pandemic influenza, such as H1N1 or others, that could emerge in future. Furthermore, there would be fewer deaths in high-risk individuals and less time lost from work and school in healthy populations.”
Farr believes the earliest we could see a universal flu vaccine approved and rolled out is Summer 2024, but this depends on the data generated from the phase I trial and completion of phases II and III. “The National Institute of Allergy and Infectious Diseases’ standards for a universal flu vaccine state that it should be at least 75 percent effective in order to greatly reduce prolonged transmission in a population,” he says. “It should protect against group 1 and 2 influenza A strains, provide durable protection for one year, and be suitable for all age groups.”
ID Transmission will, of course, keep you updated on clinical trial progress.
Reference
- National Institutes of Health, “Clinical trial of mRNA universal influenza vaccine candidate begins” (2023). Available at: bit.ly/4282yz2.