A Question of Efficacy
Assessing immunogenicity of the MVA-BN vaccine against mpox in humans
Up until May 2022, mpox primarily occurred in western and central Africa. When widespread reports started to roll in about cases in non-endemic countries, we saw a shift in the global health response against the disease and, two months later, the Director-General of the World Health Organization declared a Public Health Emergency of International Concern. The world was still reeling from the effects of COVID-19 – the desperate race for a vaccine fresh in most people’s minds – so the existence of a licensed poxvirus vaccine approved and in use for smallpox and mpox was in stark but welcome contrast.
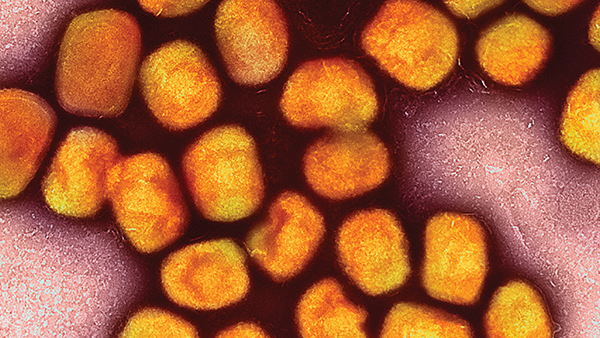
Approved for mpox in the US in 2019, the modified vaccinia virus Ankara-Bavarian Nordic (MVA-BN) is a third-generation smallpox vaccine based on an attenuated strain of the vaccinia virus. Mpox is a member of the Orthopoxvirus genus and related to the Variola virus, the cause of smallpox; therefore, the vaccinia virus is used for smallpox and mpox vaccine formulations because of the cross-protective immunity to orthopoxviruses.
However, one problem remains, say Luca Zaeck and Corine Geurts van Kessel from the Erasmus University Medical Center. “Although MVA is licensed as a vaccine in humans against mpox in Canada and the US and approved by the European Medicines Agency under special circumstances, there was virtually no efficacy or immunogenicity data of the vaccine against mpox in humans available.” They continue, “Efficacy of MVA in humans against smallpox has been inferred based on non-inferiority of immunogenicity in clinical studies and cross-reactivity against mpox has been assumed due to protection of non-human primates against severe disease in animal trials.”
Zaeck, Guerts van Kessel, and their team felt compelled to address the knowledge gap and provide researchers with a tool to measure mpox-specific immune responses – keeping three crucial questions in mind (1).
- Does historic smallpox vaccination induce antibodies that are cross-reactive with mpox?
- Do individuals with mpox rapidly mount neutralizing antibody responses?
- Does MVA-BN vaccination induce MPXV-reactive and neutralizing antibodies?
MPXV-neutralizing antibodies were detected post-vaccination and infection. Individuals receiving only the two-dose MVA-BN series without historic vaccination exhibited relatively low MPXV-neutralizing antibody titers, but those with a history of smallpox vaccination or after mpox infection had higher titers. “Vaccine-induced immunity after historic smallpox vaccination was long-lasting and cross-reactive,” say Zaeck and Guerts van Kessel. “MPXV-neutralizing antibodies were found in individuals even 70 years after their vaccination; however, although MVA vaccination induced a general poxvirus-specific antibody response, the levels of cross-reactive MPXV-neutralizing antibodies following the two-shot regimen were comparatively low.”
Using an MVA-based influenza vaccine, they further showed that dose-sparing led to lower MPXV-neutralizing antibody titers, but a third booster dose significantly enhanced the cross-reactive MPXV-neutralizing antibody response. The research provides insight into the immunogenicity and cross-reactivity of MVA vaccine-induced immunity and provides a foundation for further work into MVA-induced MPXV-specific immune responses.
But there is still work to be done – and a lot left to learn about the protective capabilities of MVA vaccination for mpox. For example, the study wasn’t intended to measure vaccine efficacy, so the protective role of MPXV-specific neutralizing antibodies after vaccination still remains unclear, demonstrating the need for cohort studies to assess vaccine efficacy in at-risk populations. “Does MVA vaccination protect against mpox infection? If not – or not entirely – does it reduce disease severity and hospitalization rate? What is the correlate of protection against mpox? What is the role of other parts of the immune system, such as the T cell response?” question Zaeck and Guerts van Kessel. “We would like to investigate this further by diving deeper into the immunological signature generated by MVA vaccination.”
Reference
LM Zaeck et al., “Low levels of monkeypox virus-neutralizing antibodies after MVA-BN vaccination in healthy individuals,” Nat Med, [Online ahead of print] (2022). PMID: 36257333.