Significant Steps for Sepsis
How an ultra-rapid antimicrobial susceptibility test could dramatically reduce diagnostic times for sepsis
Sepsis affects over 40 million people around the world each year, and it has an extremely high mortality rate – 20–50 percent – meaning that more than 10 million people can die from sepsis annually. To reduce this mortality, it is crucial to quickly diagnose and administer optimal antibiotics to the patients. Enter a team of researchers from Seoul, Korea, working on a rapid-diagnosis sepsis test.
We spoke with Tae Hyun Kim, one of the lead researchers on the “Blood culture-free ultra-rapid antimicrobial susceptibility testing” study, to learn more.
What inspired your study?
The current hospital protocol for determining the appropriate antibiotic, known as antibiotic susceptibility testing (AST), typically takes 3-4 days. This waiting period could make the difference between a successful or fatal case and, as engineers and life scientists, we needed to do something about it. To understand why AST takes so long, we had to examine the workflow and procedures carried out in the hospital.
AST is composed of a series of complex microbiological procedures:
- Blood culturing to detect and grow the pathogens present in the blood.
- Purifying the pathogens from other blood components.
- Identifying the type of pathogen.
- Testing which drugs the pathogen is susceptible to.
- Additional steps like cell counting and gram staining.
To expedite the lengthy traditional AST process, many research groups have developed a rapid AST (RAST) method, which eliminates the purification procedure, and shortens the entire process by 20-40 hours. Despite these advancements, the requirement for blood cultures, which takes at least a day, remains a significant hurdle.
We sought to overcome this limitation by developing an integrated technology capable of completing all necessary AST testing steps in a single day without the need for blood cultures.
What challenges did you overcome during this research?
We faced numerous challenges in our research, as we aimed to develop cutting-edge technology that could make a significant clinical impact in hospitals. Unlike other studies that focus on improving just one step of the diagnostic process, our goal was to create a comprehensive solution that could transform how doctors prescribe antimicrobial treatments, especially for sepsis patients.
We wanted to combine all the key steps of AST – pathogen isolation, fast cultivation, identification, and drug susceptibility testing – directly from blood samples. To achieve this, we had to carefully design and optimize each step to function seamlessly together. This involved a lot of trial and error, especially when testing with different bacteria, to make sure the system performed consistently and met hospital standards.
We also worked closely with physicians to understand the practical requirements for real-world use. By observing hospital diagnostic procedures, we continuously improved our platform’s design. Though this project took a lot of time and effort, we believe our commitment to integrating new technologies at every step made this breakthrough possible.
How does your method work?
Our ultra-rapid AST (uRAST) assay operates through the following steps:
1) Isolating pathogens: We use nanoparticles coated with beta-2-glycoprotein 1 peptides (β2GPI-nanoparticles) that attach to a wide range of pathogens without binding to blood cells. A magnetic field is then applied to separate the blood components, leaving behind pure pathogen samples. These samples are then used for both (2A) species identification and (2B) drug susceptibility testing at the same time.
2A) Species identification (QmapID): Part of the isolated pathogen sample is used to identify the type of bacteria. Our test uses microdiscs with unique patterns and DNA probes that detect specific bacteria. When a pathogen’s DNA binds to the correct microdisc, a fluorescent marker is added, which helps identify the bacteria by reading the microdisc’s pattern.
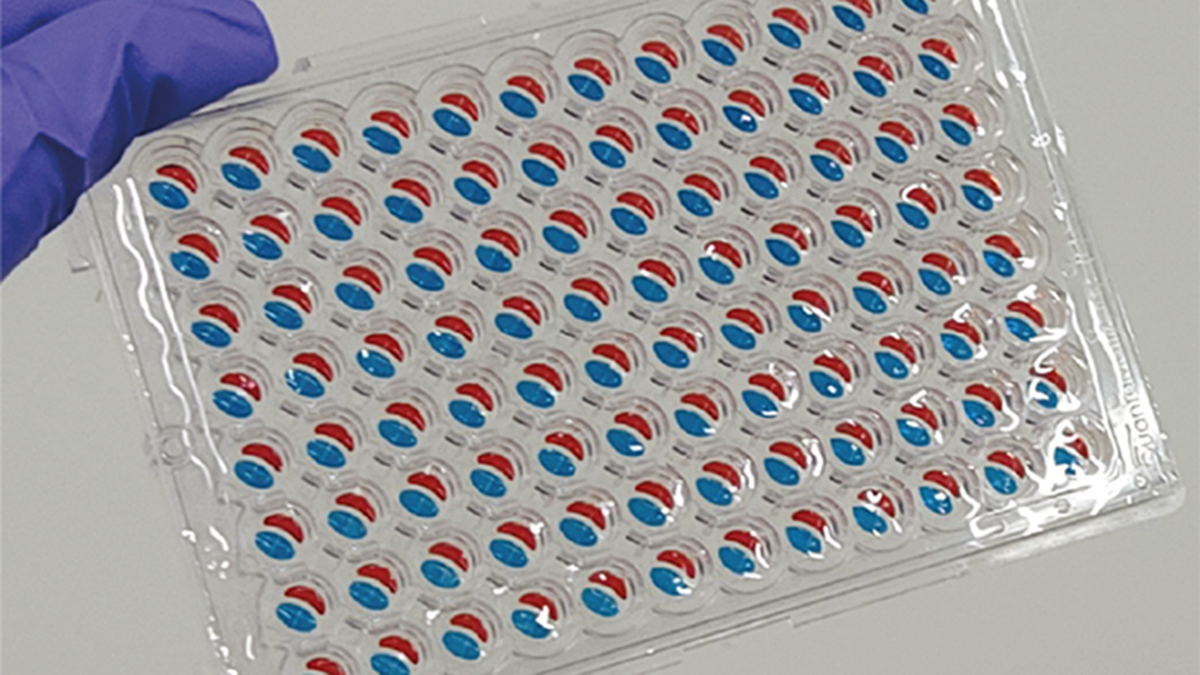
2B) Drug susceptibility testing: Meanwhile, the pathogen is cultured in a special liquid that speeds up bacterial growth. After a few hours, the bacteria are placed into wells on a microfluidic chip, each containing different antibiotics. We monitor the bacterial growth using time-lapse imaging to determine which antibiotics are effective.
By integrating and streamlining these steps, we have developed the fastest method for this testing process.
What types of infections could benefit most from this method approach?
In this study, we focused on bloodstream infections caused by bacteria because they can benefit the most from our technology. However, our approach could also transform AST for fungal infections. Patients with fungal sepsis face higher death rates because fungal cultures take even longer than bacterial ones. By adjusting our platform to meet the needs of fungi, we aim to continue our research and provide an effective solution for these challenging cases.
Do you think this method could be easily adopted in hospitals and clinics? What challenges might there be in wider implementation?
Unfortunately, despite significant technical advancements, even RAST methods developed over a decade ago have yet to see widespread adoption in hospitals. One of the main barriers is the stringent yet somewhat outdated regulatory standards, which are still based on traditional AST methods and don’t fully understand the benefits of newer technologies like ours. Additionally, new technologies must undergo strict clinical evaluations to get approval and insurance coverage, which is a slow and difficult process for companies. Introducing new technology could also create uncertainty as they require hospitals to reorganize roles, train staff, and change workflows, which many are hesitant to do.
Despite these hurdles, we believe that the uRAST system has the potential for widespread implementation in the near future. To facilitate this, we’re developing an automated device that can perform all the tests, simplifying the process and reducing the need for staff training. By automating procedures, we aim to reduce delays and increase the system’s clinical impact.
Our team has dedicated over a decade to AST research with the goal of saving lives in hospitals. During our clinical pilot study, we saw many sepsis patients lose their lives, which strengthened our commitment to this cause. Our goal extends beyond academic achievements; we aim for the successful implementation of our technology in hospitals, where it can truly make a life-saving impact.
How do you see this method influencing future diagnostic practices, especially in the fight against antibiotic resistance?
Antimicrobial resistance is a significant global threat, largely fueled by the unnecessary use of broad-spectrum antibiotics. Because current AST methods take too long, healthcare providers often give broad-spectrum antibiotics as a precaution. It is estimated that 14–78 percent of antibiotics prescribed are unnecessary or ineffective, exposing pathogens to treatments that don’t work and speeding up the development of resistance.
This delay in diagnosis directly contributes to the rise of antibiotic-resistant bacteria. As resistance increases, standard treatments become less effective. The World Health Organization predicts that by 2050, antibiotic-resistant infections could cause 10 million deaths each year.
Developing new antibiotics is difficult, with few new drugs in recent years. Therefore, we need to treat existing antibiotics as a valuable global resource and minimize unnecessary use to slow down resistance.
Our uRAST method offers a solution by helping healthcare providers quickly identify the right antibiotic, reducing the need for broad-spectrum drugs. This approach can help prevent antibiotic resistance, preserve current antibiotics, and support better antibiotic use.